Introduction
On 7 November 2024, a consultant told me I was “Stage IV – Incurable, Inoperable; palliative care only.” Those words weighed heavier than the 9.2cm tumour in my oesophagus.
If you’ve never sat in a cold consulting room and heard those words (and I truly hope you haven’t and never have to), let me explain: it’s not just a medical statement. It’s a subtle way of saying this road ends here. Some accept that. But for others (like me), “palliative” isn’t the end; it’s just the beginning of a different path.
This post isn’t about denial or false hope. It’s about understanding what “palliative care only” really means and why stopping there could take away options that can change outcomes. It’s also about how I turned that moment into a turning point that saved my life – at least long enough to write this, 1 week after the passing of my prognosis.
What “Palliative Only” Really Means
“Palliative” comes from the Latin word palliare, which means to cloak. In oncology, it refers to treatments aimed at easing symptoms, improving quality of life, and possibly slowing progression – but not curing. That distinction is important. I also want to note here; Incurable also doesn’t mean untreatable. Yet too often, the shorthand “palliative care only” gets taken as: there’s nothing more we can do – get your affairs in order.
The issue isn’t bad doctors; it’s a strained system, pressed by time constraints, guidelines, and outcomes data. When a patient hears “palliative care only,” it can crush hope and curiosity in a heartbeat. That’s dangerous. Agency – the drive to ask, to question, to explore – is often the one medicine no one can prescribe, yet it can change everything.

My “Palliative Care Only” Moment
My own “palliative care only” moment came 3 days after my mother passed away and only a few weeks after my partner Ana had half her lung removed for her own fight with cancer. The timing was cruel.
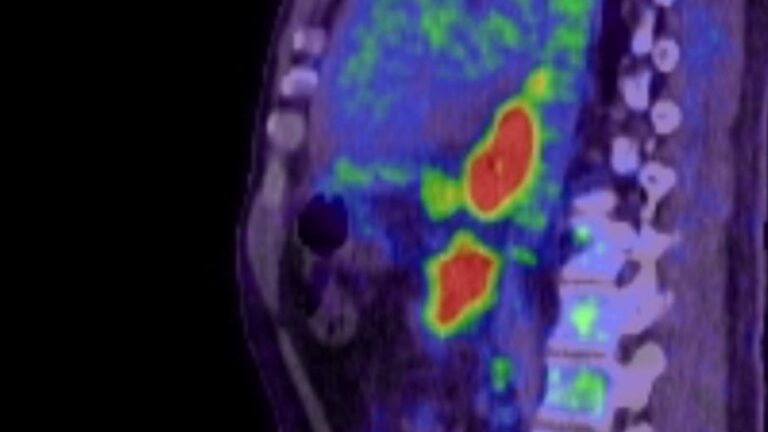
The consultant was brisk and efficient. The PET scan showed a 9.2cm oesophageal adenocarcinoma, extensive retroperitoneal lymph node involvement, a secondary on my aorta (and we’ve since discovered there may have been another on the neck of my pancreas also). Surgery was not an option. “Inoperable. Incurable. Palliative care only.”
I remember walking out of that room feeling numb, as if my body had already accepted the death sentence my mind hadn’t processed yet. I recognised the irony: here I was, a compliance officer by trade, caught off guard by life’s fine print.
But grief quickly turned into something else: defiance. If the road ended here, I would build a new one.
Finding the Fork in the Road
So I did what I’d always done in business: treated cancer like a criminal I was hunting through the financial system. If the system wanted to write me off, I would audit the system, build a process and find a way to systemise and beat it at its own game.
I took practical steps first:
Second opinions. I reached out to Dr. Thomas Seyfried – Professor of Biology, Genetics & Biochemistry at Boston College; Dr. Andy Gaya – GI oncology specialist at the Cromwell hospital in London; Dr. Elizabeth Smyth – Oncologist and Researcher at Oxford University Hospital; Dr. Isabella Cooper – Metabolic Researcher at the University of Westminster; and others. Fresh eyes can bring different ideas.
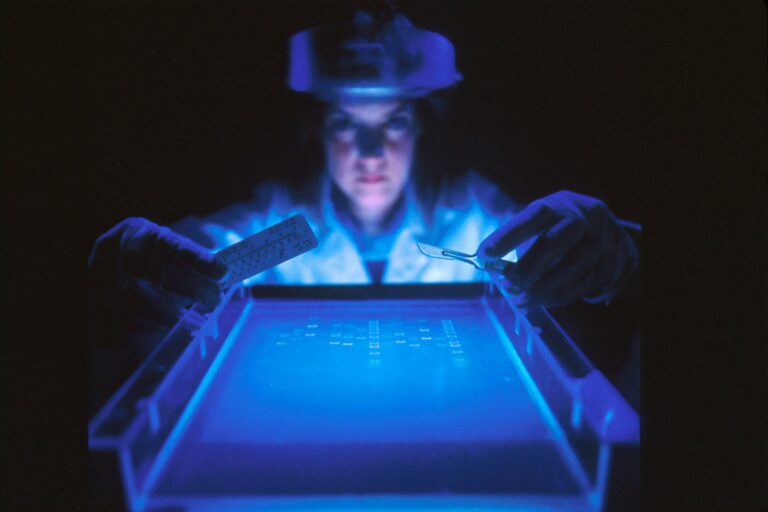
Next-generation sequencing. If cancer had mutations, I wanted to know their playbook.
Learning from outliers. Books like “How to Starve Cancer” by Jane McLelland, “Radical Remission”” by Kelly Turner, and “Cancer as a Metabolic Disease” by Thomas Seyfried presented strategies outside the standard protocols.
This wasn’t about rejecting the NHS. I’m alive partly because of what they did. It was about adding to their map with routes they didn’t have time, funding, or permission to draw.

Off-Label Medicines and Integrative Tools
Here’s where the fork became a new road. With support from forward-thinking doctors and countless hours on PubMed, I created an off-label and integrative protocol.
Off-label medicines* (those used for purposes other than those for which they were approved):
• Metformin – Lowers glucose and insulin availability; disrupts tumour energy supply
• Pantoprazole – Alters tumour pH; may help make chemotherapy more effective
• Ivermectin – Interrupts cancer cell metabolism; suppresses WNT signalling
• Fenbendazole – Disrupts microtubules and glucose metabolism
• Mebendazole – Similar to fenbendazole; also blocks angiogenesis
• Sulfasalazine – Inhibits xCT transporter; impacts glutamate signalling and detox mechanisms
• Propranolol – Blunts stress hormones that fuel tumour growth and vascularisation
• Aspirin – Anti-inflammatory, anti-platelet; may reduce metastasis
• Celecoxib – COX-2 inhibitor; targets inflammatory pathways
• Cimetidine – H2 receptor blocker; may reduce immune evasion and cancer cell adhesion
• Doxycycline – Targets cancer stem cells; disrupts mitochondrial function
• Itraconazole – Blocks angiogenesis and Hedgehog signalling
• Hydroxychloroquine – Inhibits autophagy; starves stressed cancer cells
*Please note: this is not my full protocol – far from it – just a snapshot of some of the prescription medicines I’ve taken over the course of my journey. I will cover each medicine individually in later posts (I also want to give Mark Duman a nod here – he’ll know why), including things to know and interactions to be aware of, etc.
Integrative tools*:
• Melatonin – not just for sleep; high doses show effects against cancer.
• Omega-3 DHA/EPA – anti-inflammatory and helps cell membranes.
• Curcumin with piperine – inhibits NF-kB and COX-2 pathways.
• Keto vegetarian diet – starves tumours of glucose while providing healthy cells with ketones.
• Fasting – makes cancer cells more sensitive to treatment.
• IV Vitamin C (at doses above 80g) – produces hydrogen peroxide that is toxic to cancer cells.
• Hyperbaric Oxygen Therapy (HBOT) – increases oxygen tension, helping counter hypoxic tumour environments.
*To be clear, this is not medical advice, just what I personally used. You should consult a knowledgeable professional before embarking on any of these for your own journey – some may be genuinely dangerous if not used correctly or with proper context
Some important first step picks for readers exploring integrative support:
– Magnesium Glycinate → Amazon link
– Vegan Omega-3 DHA/EPA → Amazon link
– Curcumin + Piperine → Amazon link
– Vitamin D3 + K2 → Amazon Link
– Berberine → Amazon Link
For me, these 5 are an essential base and first step in any off-label protocol. I’ve added links to the best versions I have found in the UK – the ones Ana & I use ourselves – (links should also work for US too, but ingredients may differ so please check before ordering) – they should contain no fillers or other unwanted chemicals.
Reframing “Palliative” Without Losing Faith in the NHS
I need to clarify: I’m not here to criticise the NHS. They saved Ana’s life, and they’ve saved mine in ways I couldn’t replicate privately. The doctors and nurses on the front lines are doing heroic work.
But systems are blunt tools. Labels like “palliative” serve as shorthand for managing expectations. Unfortunately, they also crush hope. And hope – combined with evidence, rigor, and agency – is not a luxury; it’s essential for survival.
“Palliative care only” should not mean “stop asking questions.” It should mean: we’ve reached the edge of our map. But there may be other paths.

Practical Steps if You Hear “Palliative Only”
Here are five things I wish I’d known right away:
– Ask better questions. “What are my options?” “What else is being trialled?” “What happens if I don’t accept this plan?”
– Seek a second opinion. Even within the NHS, consultants may interpret the same scans in different ways.
– Explore metabolic health. Diet, exercise, sleep, and stress are areas you can control.
– Read the right books. Start with “How to Starve Cancer” by Jane McLelland, “Radical Remission”” by Kelly Turner, and “Cancer as a Metabolic Disease” by Thomas Seyfried.
– Consider supplements carefully. Evidence-based basics like omega-3, vitamin D, and magnesium are safe starting points – but always check for interactions.

Conclusion
Being told you are “palliative only” can feel like a death sentence. For me, it is the most dangerous word in oncology – not because it was untrue, but because it was incomplete.
Those two words nearly shut down the fight before it began. Instead, they pushed me to build my own road. That road is messy, unproven, and tiring. But it’s still a road, and I'm still on it, and nearing NED (No Evidence of Disease) now…
If you or someone you love hears “palliative only,” pause. Don’t give up your agency to two words. Ask another question. Get another opinion. Keep searching.
Because sometimes the strongest medicine is simply refusing to accept that the map ends where someone else says it does.
Subscribe to stay connected