Prologue – Grief Arrived Before the Staging Report Did
My mum died on 27th October 2024.
We got the news the next morning, 28th October – which was also Axel’s (the elder of my two boys) 3rd birthday. There’s something truly absurd about blowing up balloons whilst also calling around relatives to tell them your mother is gone.
The kitchen smelled like pancakes and grief. Amid the candles and wrapping paper, my phone lit up with a call from Gill, one of my mum’s oldest and closest friends', and executor on her estate. She was doing her job, sounding brisk and practical as people often must in tough times. I answered because that’s what you do. You keep moving. You keep choosing. You make lists while your chest feels heavy. In all honesty, I thought she was just ringing to pass on her apologies for my diagnosis – never in a million years did I think she was calling to tell me my mum was dead.
By then, I’d had the CT and endoscopy – on my youngest’s 1st birthday. I’d watched the consultant react with that soft professional “oh” and heard the word malignant. The CT scan had already suggested the worst, my weight loss proved it, and the back pain – pressure from the tumor pressing on a nerve cluster – had screamed for attention. Mum’s death didn’t start the avalanche; it just sped it up.

31st October – The Room Where “Incurable” Entered the Chat
Three days after Mum died, I sat in a clinic room with Mr. Booth at Bracknell Health Centre and heard the formal words: inoperable, incurable, palliative only. Surgery was not an option. It had spread to nodes you don’t argue with, the ones tightly wrapped around the body’s main trunk line. He was careful, humane, and precise. It was a type of clarity you can’t unhear. In all, the meeting lasted less than 3 minutes – Ana didn’t even have a chance to wipe her tears before we were ushered out the room.
I don’t remember much about the furniture or the art on the walls, but I remember the air felt thin and the clock ticked loudly. I remember how clinical language can be both a mercy and a weapon. As I left, I thought: This must be what it’s like to be told the building is on fire and then handed a glass of water.
We confirmed the PET scan for the next day – 1 November to confirm what the CT had hinted. I nodded as if I still understood this language.
Ana’s parents flew back to Texas on 4th November. We hugged them goodbye at the Heathrow drop off. They had come to take care of their daughter after a lobectomy, and left seeing their son-in-law face a terminal prognosis. Life doesn’t follow a neat path.
The Week After the Endoscopy – Guernsey, a Sauna, and an Idea
In the middle of everything, I drove to Guernsey to pick up a sauna from my dad’s storage. People might think: A sauna? Now? Yes, now. When your nervous system is on edge, heat and sweat can feel like a small act of rebellion – a place where your body is still yours.
On the ferry, I listened to an episode of Steven Bartlett’s Diary of a CEO, the one with Professor Thomas Seyfried discussing the metabolic theory of cancer. It was half hope, half research. He spoke about mitochondria, glucose, ketones, and how tumors cheat the rules – ideas that made sense to my brain. The ship sliced through a grey sea, and I decided to email him. If the house is burning, you don’t debate which hose to use.
He replied within hours. He introduced me to Dr. Isabella Cooper at the University of Westminster – a brilliant metabolic researcher who, in those early weeks, was exactly the kind of person I needed: smart, grounded, not easily impressed or dissuaded. She didn’t promise miracles. She talked about mechanisms and probabilities. It felt like breath. She gave me sanity and something to focus on.
At home, I started reading as if my life depended on it – because it actually did. Jane McLelland’s How to Starve Cancer. Kelly Turner’s Radical Remission. A few others , all with dog-eared pages and coffee stains, already… Not scripture – just guides. Not instructions – just options.

18-19 November – Two Days That Redrew the Map
18th November was Mum’s funeral. I had to leave early. I hated that I did it, but I had to. The next morning, 19th November, the day before my 36th birthday, I had my first meeting with Dr. Esme Hill, my NHS oncologist. It was the earliest slot they had available. Grief and triage had to share a calendar.
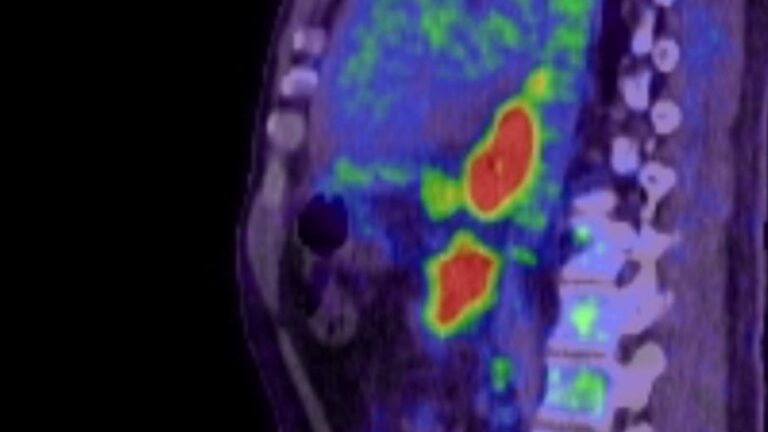
That morning, I walked into the clinic with two things: a folder of notes and the PET results hanging over me like dark clouds. Dr. Hill was direct, which I appreciated. She told me what the scan showed: a large, deeply FDG-avid primary tumor with metastatic spread to multiple nodes and other sites too, including the para-aortic chain. She explained what it meant in NHS terms: Palliative only.
There it was – the phrase everyone knows but no one wants to hear: Palliative only. I nodded. I asked questions. I was polite. For a moment, I was someone different – a man who could handle this without breaking down.
We discussed options – or the lack of them – and what “palliative” really means: managing symptoms, treatments to extend life and ease the path, not cure it. We talked about chemo, timelines, side effects, and logistics. I listened. And somewhere in that practical, compassionate conversation, I had the quiet thought I’d been circling since the endoscopy:
I hear you. I respect you. I’m not stopping here.
This isn’t a criticism of Dr. Hill or the NHS. They saved Ana and would later help me through some tough months with care and professionalism. But there’s a difference between being told you are palliative and deciding you will live that way. One is a medical label; the other is a choice. I can accept the first without agreeing to the second.
I left the clinic, sat in my car, and let out a long, heavy breath – It must have taken me a good ten minutes to come back into myself. Then I drove home to a kitchen still filled with deflating balloons from two kids' birthday parties and a family calendar covered in appointments that couldn’t care less about my feelings.
Happy almost-birthday, Dale.

Dark Wit, Because What Else Do You Do?
There’s a joke I keep telling myself that isn’t funny: I started a business, and cancer started one too. Mine was a consultancy. Cancer’s was a hostile takeover.
Everything in business ultimately boils down to persistence and/or consistency – this was no different. Me vs Cancer – who was going to be the more persistent and consistent…
I was supposed to be in a suit, discussing a very significant transformation program with a high-street bank on 17th October. Instead, I was in Somerset, telling my mum she was right to worry. In another life, the bank signed with someone else and celebrated. In this life, I took a ferry to get a sauna and emailed a scientist about starving tumors.
There’s a version of me that might have felt embarrassed by that, and all of this. To whom the thought of sharing any of this would be the furthest thing from my mind. But that person is long gone now.
The Clinical Bits (Summarised, Because You Asked)
13 Oct – CT Scan
15 Oct – Endoscopy: malignant-looking mass in lower esophagus, biopsied.
31 Oct – Surgical consult (Bracknell): inoperable, incurable, para-aortic nodal involvement suspected; PET scan booked.
1 Nov – PET scan (FDG): large avid primary, multiple nodal metastases including para-aortic chain.
11 Nov – Started HBOT (hyperbaric oxygen therapy) as part of an integrative protocol.
18 Nov – Mum’s funeral.
19 Nov – First oncology consult (Dr. Esme Hill): PET results reviewed, palliative only; discussed chemo and supportive options.
21 Nov – Booked my first session with Amanda King – Naturopath and Nutritionist
Everything else in between was a blur of paperwork, childcare, numbers, and sleepless nights.

What Grief Did (Besides Everything)
Grief rearranged the furniture in my head. It made small talk impossible and silence unbearable. It made kindness feel like a conspiracy and competence a miracle. It slowed me down while the world sped up. It also took away any lingering caution. When someone you love dies whilst you wait for a scan result, any patience you had for being “reasonable” vanishes.
I don’t mean I acted recklessly. I mean I became clear. If a therapy had physiological sense and manageable risks, it went on the list for testing. If it didn’t, it didn’t. Mechanisms before marketing. Physiology before forum posts. If two experts disagreed, I read the research, asked better questions, and tried not to become overly devoted to any one approach.
That’s when my protocol began to take shape – not as a monument to hope, but as a plan. Metabolic focus first. Nutrition I could stick with (vegetarian keto, tightly controlled). Off-label medications backed by data and prescribed by a truly knowledgeable integrative oncologist. HBOT sequenced thoughtfully. Tools for my nervous system (red light therapy, PEMF, breathwork) because they didn’t cure cancer, but helped me manage the hard choices ahead.
I wasn’t rejecting the NHS. I was refusing to outsource my survival.
A Note on “Palliative Only”
“Palliative only” broke my heart like a clean break: painful, swift, and healing set on the wrong angle if not reset early. It describes treatment intent, not what you can attempt. It says, “we cannot cure this with the tools we have,” not “you cannot change your situation.”
If you’re reading this from the perspective of that same phrase, I can’t promise anything. I won’t. But I can say intent matters – both theirs and yours. I can say a system designed to measure cures may overlook other victories: energy, time spent with your children, reduced suffering, increased resilience, and regained capacity. These are not consolation prizes; they are the fabric of life.

The Quiet Line I Drew
Leaving Dr. Hill’s office, I set three simple rules:
Evidence over ideology. If something has plausible mechanisms and reasonable safety, it’s worth examining. If it’s a trendy meme with a brand, probably not.
Add slowly, measure honestly. Make one change at a time where possible; no fairy-tale thinking when I don’t “feel” something.
Keep living. Exercise as medicine. Breathwork every morning. Family first. Laugh when I can. Cry when I must. Sleep like it’s therapy (because it is).
These aren’t heroic rules. They’re mundane. That’s the point. Cancer is chaos. Boredom is a survival skill.
What I Did Next (Preview)
I drove to Guernsey for a sauna because regulation beats rumination.
I listened to Seyfried, contacted him, and connected with Dr. Isabella Cooper, who helped me cut through the noise.
I read McLelland and Turner along with a stack of papers, and began sketching a metabolic protocol that made sense for my tumor.
I started HBOT on 11 November, the week before my mums funeral, because oxygen, sequencing, and physiology aren’t fads – they’re tools.
I kept loving my children as if there were no prognosis. Because for them, there isn’t.

Closing. The Day I Refused “Passive”
If Part 1 of my story was the fortnight everything fell apart, this is the week it stopped falling. Not because the news got better – it didn’t. But because I did. I transformed from someone waiting to be told what to do next into someone deciding what to try next – respectfully, relentlessly, within safe bounds, outside the lines of resignation.
“Palliative only” may be a medical classification, but it isn’t a way of life.
Subscribe to stay connected




Thank you for your open and vulnerable sharing. I am a bereavement counselor that has spent years walking with the ill and dying. You have an unbelievable story, mixed with dark humor (a necessity!) and great character. I pray that you will keep living your best life in the midst of this dichotomy of gratefulness and gut-wrenching pain. What an unbelievable honor to hear your story.
Keep pushing ahead in the way only you can and will do.
Blessings to you-
Thank you so much for your kind words Rani – and for the work you do. My mum was a palliative care nurse, so I’ve seen first-hand the emotional weight and compassion that a role like yours requires, and I applaud you for it. It’s not an easy path, and it takes a special kind of person to do it with heart.
You’re right about dark humor — it’s one of the few tools that makes the unbearable even slightly manageable. I’m really grateful that what I share resonates, and that people like you connect with it from such a place of understanding.
Thank you again — for your empathy, your encouragement, and for showing up for so many when it matters most.